The Diagnosis of Osteo-arthritis
The diagnosis
Osteoarthritis (OA) is a chronic joint disease that requires a careful approach for its diagnosis.
Traditionally, the diagnosis of OA is based on a combination of clinical assessment, the patient’s medical history, and radiographic investigations.
However, the complexity of OA and its evolution over time necessitate a detailed understanding of the various aspects involved in the diagnosis.
Clinical evaluation
and medical history
The diagnosis begins with a thorough medical history and physical examination.
The physician will collect information regarding symptoms (such as pain, morning stiffness, and functional limitation), their onset, and their progression.
The physical examination may reveal signs such as joint crepitation, swelling, and reduced range of motion.
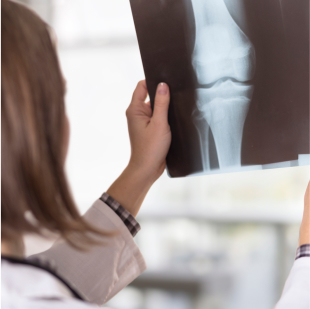
Imaging
Radiographic examination is considered the gold standard in the diagnosis of OA, allowing for the visualization of the disease’s typical features that change according to the progression of the disease, such as:
- Reduction of joint space: indicative of cartilage wear.
- Osteophytes: bone growths at the edges of the joints.
- Subchondral sclerosis: increased bone density beneath the cartilage.
- Subchondral cysts: fluid-filled cavities in the subchondral bone near the cartilage.
The most used classification system for assessing the severity of OA in radiographs is the Kellgren-Lawrence (K/L) method.
This scoring system classifies OA into five levels from 0 to 4, defining OA based on the presence of defined osteophytes (grade ≥ 2) and additional joint alterations.


Additional
Diagnostic Tests
Other imaging methods, such as ultrasound and magnetic resonance imaging (MRI), can provide additional details about the condition of the cartilage, the presence of synovial effusion, and other soft tissues involved, although they are not always necessary in routine clinical practice.
BIOMARKERS
European researchers are working to identify genes and biomarkers and promise to offer non-invasive methods for diagnosing the disease and monitoring its progression.
These biomarkers may include molecules present in the blood, urine, or synovial fluid that reflect the processes of cartilage degradation and joint inflammation.
The diagnosis of osteoarthritis requires a holistic approach that considers both clinical symptoms and instrumental evidence.
Radiographic assessment plays a key role, but the patient’s medical history and physical examination are essential for a complete diagnostic picture.
Further developments in the field of biomarkers and imaging techniques could significantly improve the accuracy of diagnosis and management of OA in the future.
Symptoms evaluation
The choice of treatment depends on various factors such as your overall health, other medications you may be taking, and the severity of your osteoarthritis—whether mild, moderate, or severe. Working with your doctor early on will help you begin a personalized treatment plan sooner.
Which therapy will work best for you?
If you are planning a visit with your doctor, you can use this osteoarthritis self-assessment tool to organize your concerns and symptoms, thus coming to the appointment well prepared.
Cristiano Sconza, MD, PhD Physical Medicine and Rehabilitation specialist Humanitas Research Hospital Milan, Italy
Symptoms evaluation tool
If you are planning a visit with your doctor, you can use this osteoarthritis self-assessment tool to organize your concerns and symptoms, thus coming to the appointment well prepared.
Cristiano Sconza, MD, PhD Physical Medicine and Rehabilitation specialist Humanitas Research Hospital Milan, Italy